This blog contains affiliate links. Read more here about what affiliatelinks are and why I use them

FODMAP diet: 100 things to know before you start
If you are feeling a bit overwhelmed by the low FODMAP diet. This blog is for you.
I have created a list of 100 helpful tips that I wish I had known when I just started this diet.
It would have made the diet easier for me to follow. And it would have helped me towards better gut health quicker.
In this blog, I have bundled all my learnings from being a FODMAP blogger for over 7 years in one article.
Let’s get going!
Table of contents
This blog contains 100 tips, so it is LONG. Use the links in the table of contents below to easily navigate to the topic you want to learn more about:
- The elimination phase
- The reintroduction phase
- The personalisation phase (after reintroduction)
- All about specific food groups
- Eating healthy
- Mindset & stress
- Relieving symptoms
- Meal planning
- Groceries & label reading
- Travelling & holidays
- Eating out
- Eating with friends & family
- If the diet doesn’t work
- The final tip
The elimination phase
1. Take some time to get familiar with the diet
Take some time to get familiar with the low FODMAP diet before starting. Get information from your dietician or doctor, read up on information online. Research which foods you can eat and which foods you should avoid. Search for low FODMAP recipes.
Starting the low FODMAP diet without preparing yourself can cause you to make mistakes and is very frustrating for yourself. Preparing yourself is the way to go 🙂
2. Get help from a FODMAP-certified dietician
The FODMAP diet is a difficult diet. It is easy to make mistakes in the beginning. It is important to make sure that you get all the nutrients you need and that you don’t stay on the strict low FODMAP diet for too long.
For that reason it is important to seek help from a FODMAP-certified dietician who can help you follow the diet correctly.
Monash University also offers a webpage where you can find certified FODMAP dieticians.
3. Beware of FODMAP stacking
FODMAP stacking is eating several foods in a meal that contain the same FODMAP group.
Individually they might be low FODMAP, but when you eat them together they might take you over your threshold for that FODMAP group. That can cause symptoms.
In this blog, I explain how to avoid FODMAP stacking.
4. Watch your serving size
The FODMAP diet is all about servings. There are a lot of foods that are low FODMAP, but only in a limited amount.
For example: eating 60 gram of zucchini is low FODMAP. But when you eat 100 gram, your serving of zucchini is high in fructans. That can lead to symptoms.
Therefore it is important to check the low FODMAP serving sizes for each food and stick to that.
Next to that, large servings of food in general and overeating can trigger IBS symptoms. Therefore it is important to not make your portions too big.
5. Make sure the information you use is up-to-date
There is lots of information about the low FODMAP diet floating around on the internet. Unfortunately, this information is not always up-to-date. There are lots of food lists with outdated information.
In general, food lists that don’t give any serving sizes for the foods listed are too general and can cause you to make mistakes on the diet. I would advise against using such lists.
Where do you go for correct information about the diet? To the creators of the diet: Monash University.
Make sure to check that the information you find online or get from your dietician is based on information from Monash University and that it has been recently updated.
Monash University is continuously doing research and information on which foods are low FODMAP and which aren’t changes often.
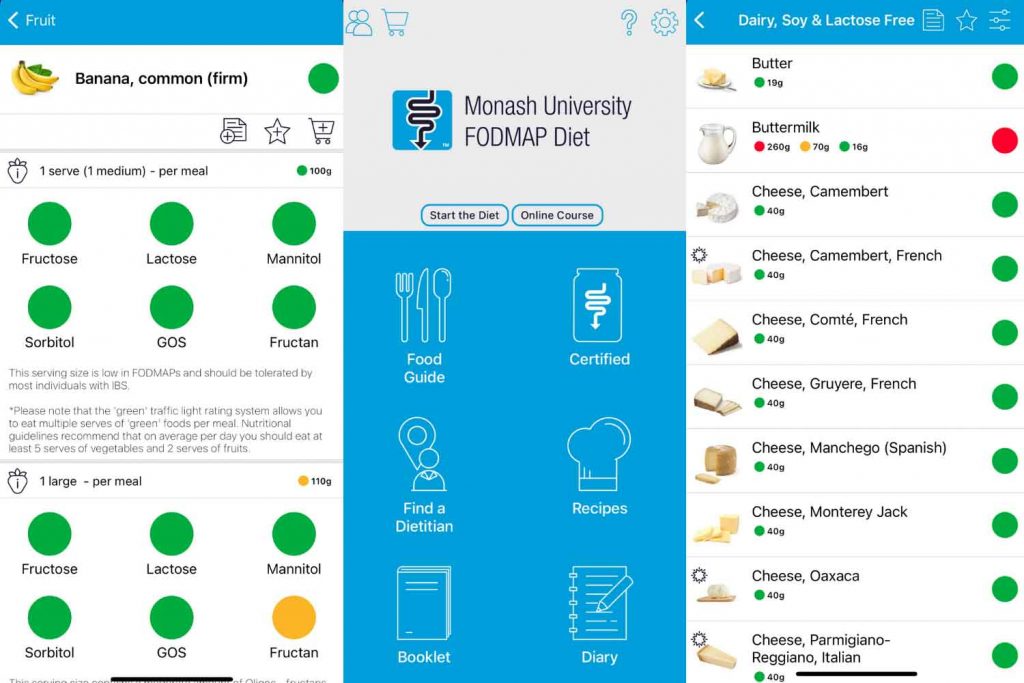
6. Use the Monash University FODMAP app
The Monash FODMAP app is the most reliable source of information for the FODMAP diet. This app is made by the creators of the low FODMAP diet and contains information about all foods that have been tested on FODMAPs.
The app shows in which amounts foods are low FODMAP or high in FODMAP and which FODMAP groups they contain. It also contains information about the reintroduction phase and recipes to help you with the diet.
With a food list that you find on the internet, you cannot be sure that the information is correct and up-to-date. With the Monash University low FODMAP app you can.
Making mistakes on the diet can influence your symptoms, therefore I advise you to use this app. You can read more about how the app works in the blog that I wrote about it.
7. Keep a food and symptom diary
It is very useful to keep a food and symptom diary during the elimination and reintroduction phase. In this diary, you write down exactly what you eat, when you eat it, which symptoms you have, and when they occur.
Writing this down can help you figure out what you are reacting to and can give you more clarity about your symptoms.
8. The low FODMAP diet is not a weight loss diet
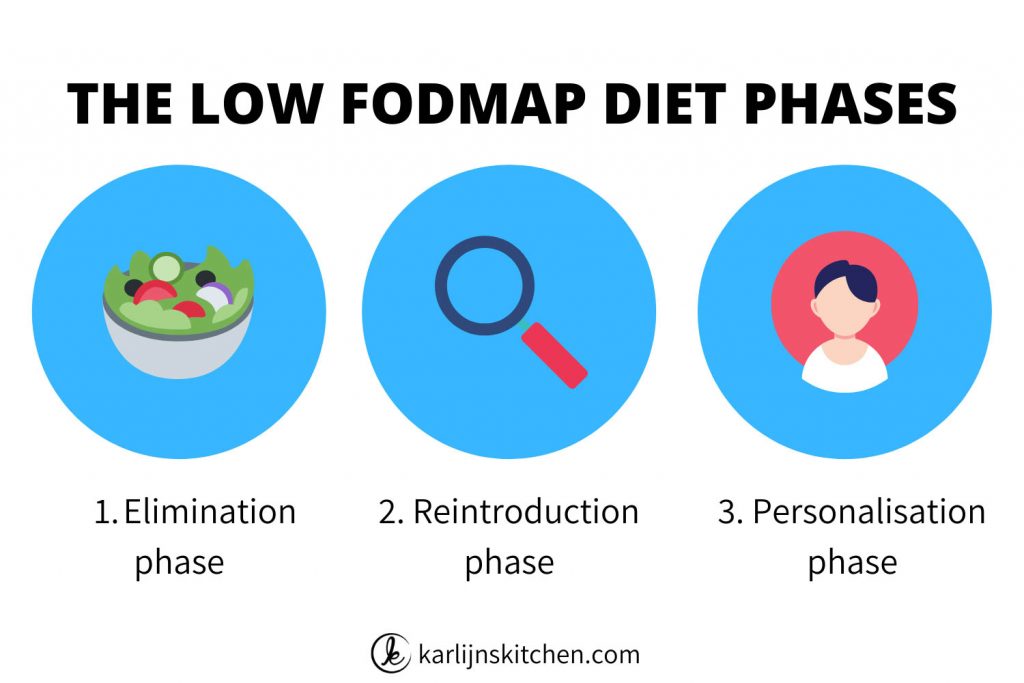
The low FODMAP diet is a diet meant for people with IBS (Irritable Bowel Syndrome). The goal of this diet is to figure out which food groups trigger your IBS symptoms.
It is an elimination diet, where you first remove several FODMAP groups from your diet and then reintroduce them back one by one to see which food groups trigger symptoms in you.
It is not a diet focused on losing weight.
9. The low FODMAP diet is not forever
The FODMAP diet is an elimination diet. You eliminate the different FODMAP groups during the elimination phase for 2-6 weeks until your symptoms settle down.
Then you start reintroducing them one by one to find which groups are your triggers.
After the reintroduction phase, you can bring the groups that you didn’t react to back into your diet. Like that, you create your own less strict personalized FODMAP diet.
It is important for your gut health to eat a varied diet that is rich in a variety of fibers.
Staying on the strict low FODMAP diet too long can negatively impact the variety of the bacteria in your gut (source).
10. Don’t stay in the elimination phase for too long
Starting the reintroduction phase can be daunting. Especially when you finally started to feel better during the elimination phase.
But for the reasons explained above it is important to not stay in the elimination phase for too long.
If you are following the elimination phase correctly, your symptoms should significantly decrease within 2 to 6 weeks, so you can start reintroducing.
11. Be patient
Even though you shouldn’t stay in the elimination phase too long, you should also give it enough time. I often get messages from people who say: “I have been on the FODMAP diet for a week and my symptoms haven’t changed.
Does this mean the diet is not working for me?”
Give it 2-6 weeks and see if your symptoms improve over that period. Some people see change in a week, for others, it takes 6 weeks.
12. What if my symptoms don’t improve?
If you have been correctly following the elimination phase of the FODMAP diet and your symptoms haven’t increased after 6 weeks.
It might be the case that your symptoms are not caused by FODMAPs. Visit your doctor or dietician to see what the next steps are that you should take.
Check this blog for often made mistakes in the first phase of the FODMAP diet.
13. Don’t over-limit your diet
The FODMAP diet is restrictive, but try to keep your diet varied within the limits of the diet.
Don’t limit yourself to only a few safe low FODMAP foods. Vary with different fruits, vegetables, nuts, seeds, grains, etc. Your gut will thank you for it.
14. Expect to make mistakes
The low FODMAP diet is a difficult diet and therefore you are going to make mistakes in the beginning. It is good to anticipate that and don’t beat yourself up for it.
There are going to be moments where you, knowingly or unknowingly, eat something that is high in FODMAPs and experience symptoms.
When that happens, don’t get angry with yourself for it. Try to have compassion for yourself and let this mistake go. For your next meal, you can make sure that it is low FODMAP again.
Working with a certified dietician can help you to avoid making mistakes. So that is highly recommended.

The reintroduction phase
After the elimination phase, you are going to reintroduce FODMAP groups back into your diet one by one. Like this, you will find out to which groups you react and to which you don’t.
15. Don’t skip the reintroduction phase
It is very comfy to stay in the elimination phase when your symptoms have settled. But please don’t skip the reintroduction phase.
It is important for your gut to be able to eat a more varied diet again after the elimination phase.
Most people don’t react to all FODMAP groups, so doing the reintroduction phase will ultimately give you more freedom in what you can eat ánd will give you clarity on which foods you should continue avoiding.
You can read more about the reintroduction phase here.
16. Eat strictly low FODMAP
Make sure to continue eating strictly low FODMAP in the reintroduction phase. The test food should be the only high FODMAP food that you are eating.
If you eat other high FODMAP foods while reintroducing, it will be difficult for you to figure out which food caused your symptoms.
17. Avoid trigger foods
If you know that there are other foods that trigger IBS symptoms in you, such as coffee or fatty foods, try to avoid them too while reintroducing.
Otherwise, they can mess with your test results.
18. Avoid stressful situations
If stress triggers your IBS symptoms, it is important to avoid stressful situations during the reintroduction phase.
If you are very stressed while testing FODMAP groups, you might not be able to distinguish whether your symptoms were caused by stress or by the food that you tested.
If you are in a very stressful situation that you cannot change, it is better to wait with the reintroduction phase or the low FODMAP diet altogether, until you are in a calmer time in your life.
19. Be careful with eating out
Be careful with eating out in the reintroduction phase because if you eat something wrong that can cause symptoms.
On days that you are testing a high FODMAP food, you can best eat only safe foods and maybe avoid eating out.
Otherwise, it will be hard to figure out if your symptoms are coming from the food that you tested that day or from other foods that you had, for example when eating out.
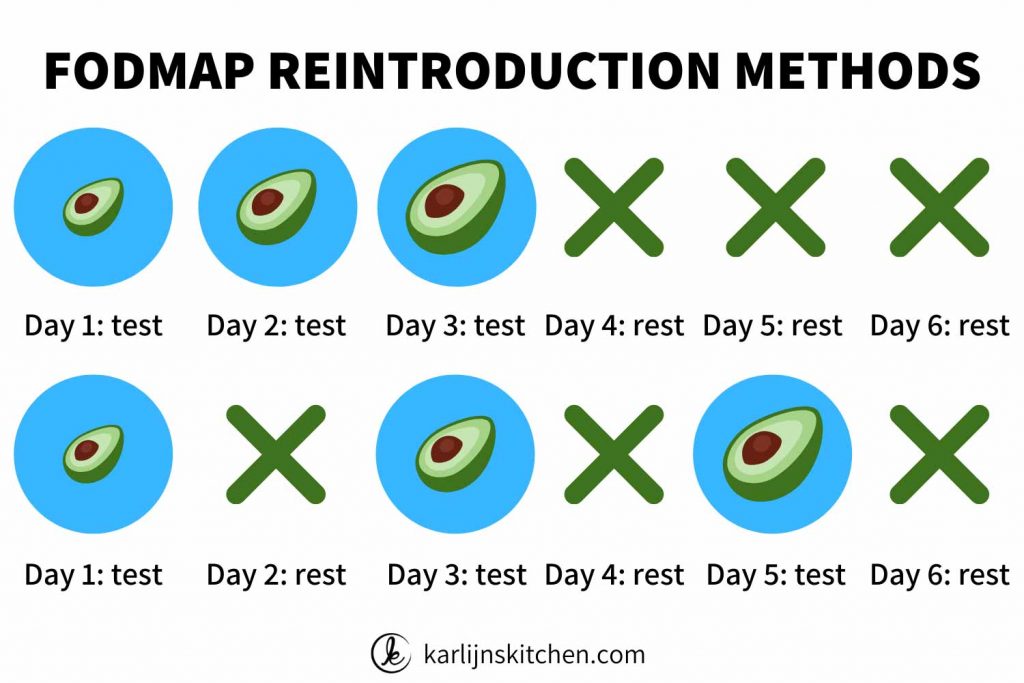
20. Pick the method that works for you
There are several testing methods. You can do three testing days in a row, but also have three testing days with a rest day between each test.
You increase the amount of the food you eat with each test.
Pick the testing method that works best for you, your dietician can help you with this. Read more about testing methods in my reintroduction phase blog.
21. Test with the right foods
Some foods are high in two or more FODMAP groups. It is important that you test a FODMAP group with a food that is only high in one FODMAP group.
For example honey is high in fructose and is suitable to test the FODMAP group fructose.
You can find more information about which foods to use for testing in this blog and in the Monash app.
In the app, open the diary, click the plus on the upper right side, and then click the symbol with the apple and the arrow.
There you can pick a FODMAP group and see which foods are recommended to test with and in which amounts.
22. Pick foods that you love eating
There are different foods that you can use to test each FODMAP group. Make sure that you use a food that you love to eat and prepare it in a way that you like. That will make testing more enjoyable.
For example: if you always eat onion fried and don’t like eating it raw, then test with fried onion as well.
Or: if you hate avocado and never eat it, then don’t use this food for testing polyols. Use a food you enjoy and will actually keep eating after the reintroduction phase.
23. Retest foods if you are not sure about your reaction
Are you not sure if you reacted to the test food or if your symptoms came from something else? Then it is best to retest this FODMAP group.
24. Reintroduce again after a year
Your gut changes, the levels of stress in your life change, and therefore your reaction to foods can also change.
For that reason, it is smart to try reintroducing the FODMAP groups that you reacted to again once a year. You might find that you tolerate them better than you did before.
25. If you have a fructose or lactose intolerance
I have a fructose or lactose intolerance, do I have to test these groups in the reintroduction phase?
No, if you were tested and the test has shown that you have a lactose or fructose intolerance, you don’t have to test these groups. You already know that you react to them.
If you were tested and the test was negative, I would test them again in the reintroduction phase. For some people, a test shows up negative, but they still find out that they react to these FODMAP groups.

26. Wait with reintroducing foods back into your diet
Wait with reintroducing groups that you didn’t react to back into your diet until you have tested all FODMAP groups.
Otherwise, the combination of two FODMAP groups might mess up your test results. After you have completed the reintroduction phase you can start to add foods back into your diet.
27. What if I react to all FODMAP groups?
If you react to all FODMAP groups, there is a chance that you have dysbiosis. This is a disbalance of the gut bacteria and because of that, your gut can be extra sensitive.
If that is the case, it is important to first focus on healing your gut and then try reintroducing again. You can find more information about dysbiosis here.
It is also possible that you have SIBO. You can read more about SIBO here.
In both cases, it is best to work with a specialized gut dietician to get diagnosed and to create a plan to solve this.
It might also be the case that something else is going on with your gut, also in that case, it is best to contact your doctor or dietician and figure out together what the next steps are that you can take.
The personalization phase
After you have finished the reintroduction phase, you can create your own personalized FODMAP diet.
You can reintroduce the groups you didn’t react to back into your diet, while you continue to avoid the groups that you reacted to.
28. Slowly add high-FODMAP foods back into your diet.
If you didn’t react to a FODMAP group, such as fructans, it is smart to add this group back into your diet slowly.
Don’t eat two slices of bread for breakfast, a meal with onion for lunch, and a meal with garlic for dinner. This will probably push you over your threshold.
Stick to the testing amount that you know you tolerate, try this at one meal, and see how it goes when you eat this food at one meal a day.
If this goes well, you can add a little more and see how that goes.
29. Test different FODMAP groups together
Monash University advises you to test the combinations of fructose + sorbitol and fructans + GOS. But only if you didn’t react to either of the groups in the combination.
In the Monash app, you can find foods that you can use to test these combinations of FODMAPs. Click Dairy, then click the plus symbol in the upper right corner, then click the symbol of the apple and the arrow.
There you can scroll down to select “fructose + sorbitol” or “fructan + GOS”.
This test will show you if you can tolerate both FODMAP groups in a meal together.
30. Test other combinations
After figuring out how much you can eat of one FODMAP group in a day, you can also start to make combinations of different FODMAP groups that you didn’t react to in a meal and see how that works out for you.

All about specific food groups
31. The FODMAP diet is not a gluten-free diet
Because fodmappers sometimes use gluten-free products, some people think that the low FODMAP diet is a gluten-free diet.
This is not the case. On the FODMAP diet, one of the FODMAP groups you are avoiding is the group fructans.
Fructans are found in several foods that also contain gluten, such as wheat, barley, and spelt. Therefore people who eat low FODMAP avoid some foods that people who eat gluten-free also avoid.
This is probably where the confusion comes from. Check out my blog Why gluten-free is not the same as low FODMAP for more information about the differences between a gluten-free and a low FODMAP diet.
32. The FODMAP diet is not a lactose-free diet
If you check the Monash low FODMAP app, you will notice that several dairy products, such as butter and different cheeses have a low FODMAP serving size.
This often leads to confusion because isn’t lactose one of the FODMAP groups that should be avoided?
Yes, lactose is one of the FODMAP groups, but the FODMAP diet is not a 100% lactose-free diet. Most people with a lactose-intolerance can tolerate a little bit of lactose.
Therefore several foods that are low in lactose have a low FODMAP serving size.
For this reason, you can eat butter on the low FODMAP diet and several kinds of cheese, such as hard yellow cheeses, mozzarella, and feta, have a low FODMAP serving.
You can read more about cheese and the FODMAP diet in this blog.
You can read more about lactose and the FODMAP diet in this blog.
Sources from Monash University: article 1 and article 2.
33. Be careful with spelt
Spelt is often recommended as a safe option on the low FODMAP diet. It is important to know that some spelt foods have quite a large low FODMAP serving, such as sieved spelt flour.
But other spelt foods are high in FODMAP or have a very small low FODMAP serving.
You can therefore not assume that every spelt food is a safe low FODMAP choice. In the Monash low FODMAp app, you can find several spelt foods that have been tested with their serving sizes.
You can read more about spelt and the FODMAP diet in this blog.
34. Be careful with soy
Just like spelt, there is often confusion about soy on the low FODMAP diet.
In the Netherlands, I often hear that people get advice from their dietician to use soy “dairy” products, while these have not been tested or are often very limited low FODMAP.
Other soy products, such as tempeh and tofu, have quite large low FODMAP serving sizes.
The low FODMAP serving size of a soy product highly depends on the processing process and therefore it is important to check the Monash low FODMAP app before using different soy products.
You can read more about soy and the FODMAP diet in this blog.
35. FODMAPs are water soluble, not oil soluble
This means that FODMAPs will dissolve in water and liquids like broth, but they won’t dissolve in oil.
If you add a piece of onion or garlic to soup, leave it to simmer, and take it out, the FODMAPs will have leached into the water. Making the soup high in FODMAPs.
If you are heating up oil in a frying pan and you add a few chunks of garlic or onion, fry it for a few minutes and take it out, the FODMAPs won’t leach into the oil. So the oil stays low FODMAP.
Like this, you can make low FODMAP garlic- or onion-infused oil to give your meal a garlic or onion flavour. Be careful with making your own garlic-oil because of the risk of botulism.
I usually just make the garlic oil that I need for the meal I am currently cooking: heating the amount of oil that I need for a recipe, adding a few cloves of garlic for a few minutes, removing the garlic, and continuing cooking my meal.
You can also buy low FODMAP garlic-infused oil or onion-infused oil, for example from the brand Fody.
The fact that FODMAPs are water soluble also causes that some canned foods are lower in FODMAPs than the same food when it is fresh.
Part of the FODMAPs in the food will leach into the water in the can, making the food lower in FODMAPs.
It is important that you rinse and drain the food well before eating it. One product that is lower in FODMAPs canned are canned mushrooms.
You can see find those canned products and the low FODMAP amounts in the Monash University app.

36. Replacing onion and garlic
Looking for replacements that will give your food an onion or garlic flavor? Try one of the following options:
Onion:
- Onion-infused oil
- The green parts of spring onion
- The green parts of leek
- Chives
- Asafoetida
Garlic:
- Garlic-infused oil
- Garlic scape powder
- Asafoetida
37. Fresh and dried herbs and spices
Do you think you can only give your food flavor with garlic and onion? Think again.
Almost all fresh and dried herbs and spices are low FODMAP and you can perfectly use them to give your meals flavor.
Just be careful with spice mixes because these often contain high FODMAP ingredients.
38. Be careful with coffee
There is no clear evidence that avoiding coffee will improve your IBS symptoms. In general, it is known that coffee can speed up bowel movement.
If you have constipation-dominant IBS, coffee might help you to get a bowel movement, but if you have diarrhoea-dominant IBS coffee might cause diarrhoea.
Because the effects of caffeine differ per person, the smartest thing you can do is keep a food and symptom diary.
If you think that coffee might trigger symptoms in you, keep a food and symptom diary for a few days.
Check if you see a pattern in your symptoms every time you drink coffee. You can ask a certified dietician to advise you on this.
Want to learn more about coffee and IBS? Check out this blog on coffee and the FODMAP diet.
39. Fat and IBS symptoms
According to this article by Monash University, we don’t know yet whether there is a cause-and-effect relationship between fat consumption and IBS symptoms. Or whether restricting fat improves IBS symptoms.
Some people see increased IBS symptoms when they consume more fatty food.
So it is good to be aware of this. If you suspect fat triggers your IBS symptoms, it is good to work with your dietician to identify what your triggers are.
40. Sugar and the FODMAP diet
I sometimes get comments that go like “How can you make a cake with sugar in it and call it low FODMAP?”
That is because normal table sugar and several other kinds of sugars are low FODMAP.
Monash University recommends not to use too much sugar because large amounts of sucrose (table sugar) may be poorly tolerated by people with IBS.
And of course, for general health reasons, it is also not recommended to use too much sugar.
But now and then a slice of homemade low FODMAP cake or some low FODMAP cookies are no problem. Isn’t that lovely!

41. Be careful with spicy food
While spicy foods like chilies are low FODMAP, they do contain capsaicin. This is the ingredient that produces the spicy effect and can trigger heartburn and abdominal pain in some people with IBS.
Therefore it is important to test how you react to spicy foods. If it triggers symptoms, it is best to limit your intake.
Source: Monash FODMAP app
42. Be careful with alcohol
Alcohol is known to irritate the gut, also in healthy people. It can affect intestinal motility, which means that it causes your food to travel down the digestive tract faster.
This can worsen IBS symptoms. Next to that, for general health reasons, it is advised to limit alcohol intake.
Not all kinds of alcohol are low FODMAP, so it is important to check what kind of alcohol you can drink. You can read more about alcohol and the FODMAP diet here.
43. Carbonated drinks can cause symptoms
There are quite some carbonated drinks that are low FODMAP, so FODMAP-wise it is no issue drinking those. However, carbonated drinks can cause bloating and gas, so it is good to be aware of that.
If you notice that your IBS symptoms worsen when you consume carbonated drinks, it might be better to avoid them.
Eating healthy
An often-asked question is: how can I eat healthy on the low FODMAP diet?
I feel like lots of healthy foods are not allowed anymore. My best tips for eating healthy on the low FODMAP diet are:
44. Try to get enough variation in your food
It is important for your gut health to have a diversified gut microbiome. Research has shown that a varied diet contributes to a diverse gut microbiome. Therefore it is important to eat a variety of fruits, vegetables, grains, nuts, and seeds.
45. Eat enough fruit and vegetables
Eating enough fruits and vegetables can feel like a challenge on the FODMAP diet, with lots of fruits and vegetables only being low FODMAP in a small amount.
In this blog, I share tips for eating enough fruit and vegetables every day.

46. Eat enough fiber
Eating enough fiber is important for a healthy gut, but this can seem like a challenge on the low FODMAP diet where lots of low FODMAP options for bread, pasta, etc. are low in fiber.
In this blog, I share tips for eating enough fiber on the FODMAP diet.
47. Healthy does not mean low FODMAP
People might ask you questions like “But avocado/garlic/onion etc. are very healthy. Why can you not eat that?”.
The low FODMAP diet has nothing to do with food being healthy or unhealthy, but with whether a food contains one of the different FODMAP groups.
You can read more about that in this blog about the low FODMAP diet.
48. Work on strengthening your microbiome
Having a healthy microbiome can improve your symptoms.
Work on strengthening your microbiome by eating enough fruit and vegetables, enough fiber, and eating a diverse range of foods. So basically by following the tips above!
49. Try to eat mindfully
Eating dinner in front of the tv, having lunch behind your laptop, and eating breakfast while you run out of the door. These are all ways to eat meals without really noticing what you are eating.
Taking time for your meals and eating them mindfully is a way to reduce stress. This can have a positive impact on your IBS symptoms.
50. Chew your food well
Chewing is important for digesting the food you eat. The smaller the food is when you swallow it, the easier it is for your body to digest.
Chewing your food well, to applesauce consistency, can also have a positive impact on bloating that you might experience after eating a meal.
You can read more about chewing in this blog by gut health dietician Manon te Linde.

Mindset & stress
Your mindset and whether you are stressed or not can also have an impact on your IBS symptoms. The tips below can help you with this.
51. Shift your mindset
People often feel overwhelmed, frustrated, and/or sad when starting the FODMAP diet: there is so much they cannot eat anymore.
I encourage you to try to look at things from a positive mindset. Look at all the foods you can still eat and the delicious meals you cán make.
Focusing on the things you can still eat will make the diet less overwhelming and will make you feel a little more positive.
There is a lot possible, even on the low FODMAP diet. Take a look at these yummy low FODMAP recipes for some inspiration.
52. Try to avoid stress
Stress can have a negative impact on IBS symptoms. Looking at which things in your life cause stress and whether you can do something to lower the stress can have a positive impact on your IBS symptoms.
A few of the tips below can also help to reduce stress.
53. Add light and medium exercise into your routine
Light and medium exercise can have a positive impact on your IBS symptoms. Exercise and moving can reduce stress and it is good for you.
You can read more about exercise and IBS here.
54. Try meditation or breathing exercises
Meditation or breathing exercises can help to reduce stress.
Taking a few minutes to meditate at the beginning and/or end of your day can help you to feel more calm, have more clarity, and feel less rushed.
If you think stress impacts your IBS symptoms, meditating might be worth trying.
You can also read this article that I wrote about reducing stress during the pandemic. Several of these tips are also useful in other stressful times.
55. Find fellow fodmappers for support
Feeling like people don’t understand what you are dealing with with your IBS and symptoms is horrible.
Even if you have people around you that are supportive, it can be very helpful to talk to people who know what you are going through.
In the Karlijn’s Kitchen Facebook Community, you can find fellow fodmappers to ask questions to, share your experience with or just get some support.

56. Be gentle to yourself
The low FODMAP diet is a difficult diet. This can lead you to make mistakes, especially in the beginning and that can also be stressful.
Try to be gentle with yourself when starting this diet. Take the diet step by step.
If you make a mistake or eat something high in FODMAPs, try to let it go and focus on eating a low FODMAP meal the next time you eat something.
Punishing yourself or getting angry with yourself when you make a mistake won’t help you and will only make you feel miserable.
The diet is not easy, making mistakes is normal. Try to remind yourself of that.
Relieving symptoms
What to do if you ate something high in FODMAPs and you are experiencing a lot of symptoms?
57. Wear comfy loose clothes
Tight clothes are not fun when you have a very bloated or painful belly. Wear comfy and loose clothing, like training pants, pants with an elastic band, pregnancy jeans, loose dresses or pajamas.
58. Make sure there is a toilet nearby
Nothing is worse than having a lot of IBS symptoms and not having a toilet nearby. If you are experiencing stomach problems, make sure you are in a comfortable situation where you can go to the toilet as often as you want and let out the trapped air in your gut.
59. Use a heating pad or hot water bottle
Some people find it comforting to have a heating pad or hot water bottle to put onto their stomach when they are experiencing a flare-up. It might not remove your symptoms completely, but it will give you some relief.
60. Make sure you eat strictly low FODMAP again
If you ate something wrong by accident, it is important to go back to eating strictly low FODMAP as soon as possible.
It is best to eat according to the elimination phase guidelines again until your symptoms settle down.

61. Try peppermint oil capsules
Some people experience relief from using peppermint oil capsules. It might be worth trying this to see if it soothes your symptoms when you have a flare-up.
Ask advice from your doctor or dietician on which peppermint oil capsules to use and how to use them.
62. Drink ginger tea
If you feel nauseous after eating something that was high in FODMAPs, drinking fresh ginger tea can help to feel better.
63. Take a walk
Light and gentle exercise can help with your IBS symptoms. It is also good to not immediately sit down after eating a larger meal but to stay standing for a while or take a small walk.
This will help your body to digest the food. Listen to your body well and only do what feels right for you.
64. Take rest
If you have a symptom flare-up, take it easy. Tell the people around you that you are not feeling well.
Follow the tips above, cancel planned activities if necessary, and take some time to rest and for your body to feel better again.

Meal planning
If you are starting out on the FODMAP diet, deciding what to eat and planning your meals can feel so difficult! These tips can help you to make it easier:
65. Create a list with your favorite recipes
Write down your favorite recipes pre-FODMAP. Go to Google, type in the name of the recipe + FODMAP, and see if you can find low FODMAP version of your favorite recipes. Then you already have a few recipes to try out.
Of course, you can also find lots of simple recipe inspiration on Karlijn’s Kitchen.
66. Make your own recipes low FODMAP
Can’t find a low FODMAP version of your favorite recipe from the tip above? Then try if you can make your own favorite recipes low FODMAP using the tips in this blog.
67. Get inspiration online
You can find a lot of recipe inspiration online. A few of my favorite websites (next to my own blog of course) are:
68. Buy low FODMAP cookbooks
If you would rather have a real cookbook instead of looking for recipes online, I would advise buying a good low FODMAP cookbook.
Not all cookbooks that pretend to be low FODMAP actually have recipes that are 100% suitable for the low FODMAP diet.
My favorites cookbooks are:
- How to make anything gluten-free – Becky Excell*
- How to bake anything gluten-free – Becky Excell*
- The FODMAP friendly kitchen – Emma Hatcher
- The gut-friendly cookbook – Alana Scott
- The 28-day plan for IBS relief – Lauren Renlund & Audrey Inouye
*These cookbooks are not 100% low FODMAP. The focus is on gluten-free recipes. But Becky has also followed the low FODMAP diet and she gives low FODMAP options for many of the recipes.
69. Try to mix things up
When you follow the low FODMAP diet, it is very easy to get stuck in eating the same meals over and over. Try to mix things up regularly by trying out new recipes.
Try some new foods as well. Open the Monash app and look for some fruits, vegetables, or grains that you hardly ever eat and search for a recipe with one of these foods.
This will make cooking more fun!
70. Take time on the weekend to plan your meals
It helps a lot if you take a moment to plan your meals for the week. Whether that is on the weekend or on Monday morning.
Sit down, grab your grocery list, favorite recipes, and cookbooks or websites, and pick out some meals for the week.
After that, you can go shopping and you will feel less lost when you are in the supermarket.

71. Make a list with replacements for products you often use
Make a list with low FODMAP replacements for products that you often use, such as grains, bread, seasonings, sauces, etc. You can find an overview of 20 low FODMAP swaps in this blog.
72. Cook for several days at once
If you feel like you don’t have enough time to cook fresh low FODMAP meals every day, you can try cooking in batches. Cook a large batch of pasta, rice, or casserole at once.
Store it in the fridge if you are planning to eat it within a few days or put it in the freezer. This saves a lot of time!
73. Stock up your pantry and freezer
Stock up your pantry and freezer with low FODMAP staples, such as gluten-free pasta, gluten-free tortillas, low FODMAP bread, low FODMAP noodles etc.
Especially if you don’t have stores nearby with low FODMAP foods, you can order online or make a trip to a store that is further away once in a while and stock up. Like this, it will be easier to create low FODMAP recipes.
74. Give FODMAP-certified foods a try
If you are not into cooking or like having a ready-made product now and then, you could give low FODMAP-certified food brands a try.
There are several brands out there where you can find low FODMAP sauces, dressings, oils, herb mixes, and more.
A few brands that I like are:

Groceries & label reading
How to go low FODMAP grocery shopping? These tips will make it a little easier:
75. Take a list of the most common high FODMAP ingredients with you
I have created a list with those ingrediënts in this blog about reading food labels on the FODMAP diet. This helps you to avoid buying foods with sneaky FODMAPs in them.
76. Take your time for grocery shopping
Plan some extra time for grocery shopping in the beginning. You won’t know what you can and can’t eat and you will have to check a lot of labels.
That takes time. By giving yourself plenty of time for shopping, you will save yourself a lot of stress.
77. Watch out for the word “spices” on labels
If spices are mentioned on a food label and they are not specified, this can mean that it includes garlic or onion. Be careful with foods like these and avoid them in the elimination phase.
FODMAP Everyday has written a very interesting article about spices and natural aromas and what they include in different countries. You can find the blog here.
In the US, for example, the word “spices” on a label cannot contain onion or garlic. But in Australia, the UK, and Europe it can.
78. Double-check food labels
Manufacturers often change the ingredients of products.
Make sure you keep double-checking food labels regularly, even if it is food that you have been using for a while or if you have read somewhere that it is low FODMAP.

Travelling & holidays
Going on holiday when you follow a restrictive diet can feel stressful. These tips will make it a bit easier for you:
79. Research the place where you are going beforehand
Google the place or area where you are going and search for things like “place name + FODMAP”, “place name + gluten-free”.
Often you will find information about restaurants and shops where you can find foods that might be suitable for the low FODMAP diet.
I usually plan ahead by looking at restaurants’ menus and checking if they have meals on the menu that might be low FODMAP or could be easily adapted to be made low FODMAP.
Creating a list of possible places to go will make you feel prepared for your holiday.
80. Make a list of translations
Going to a place where they speak a different language? Write down translations of the foods you have to avoid most.
I always bring a translation for “gluten-free” (I find that easier to explain than fructans), “lactose-free”, “onion” and “garlic”. Because these are the things that I react the most to.
In this blog, you can find translations for these words in several languages.
81. Bring an emergency food stash
If you are not sure about the availability of low FODMAP foods in the supermarkets on your holiday destination, you can bring an emergency food stash.
I always like to bring: low FODMAP bread, crackers, gluten-free pasta, noodles, and snacks.
82. Pick the right accommodation
Take some time thinking about the right accommodation for you. Personally, I don’t like being in an all-inclusive hotel where all the food is prepared for me.
Not because I don’t like eating there, but because I know my stomach won’t handle that well.
Therefore, I often pick an accommodation like an Airbnb or a hotel room with a kitchenette, where I have the option to prepare some of my meals myself. I also often take a plastic box with me and some travel cutlery, so I can quickly prepare an easy meal, like a salad.
This helps me to keep my stomach calm and to have a holiday with less food stress.
83. Prepare food for the trip
Prepare some food for the trip to your holiday. On gas stations, airplanes, and airports it is often hard to find low FODMAP options, so bringing your own low FODMAP foods will help.
I have shared some tips for low FODMAP foods to bring on an airplane here.
84. Don’t forget to keep eating fruits, vegetables, and other fibers
When you are on holiday, you often eat differently than at home. This can cause stomach problems.
Try to continue to eat fruits, vegetables, and other healthy fiber-rich foods when you are on holiday. This is good for your gut and can help your gut motility.

Eating out
How to navigate eating out on the low FODMAP diet? These are my tips for that:
85. Check the menu online
My first step is always to check the menu online. Some restaurants are just difficult when it comes to low FODMAP options.
By checking the menu online, you can figure out whether the restaurant has some options for you or not.
86. Call the restaurant to see what the options are
After picking out a restaurant, give them a call and tell them what your most important intolerances are.
I usually tell them I am intolerant to gluten (that is easier to explain than fructans), lactose, onion, and garlic and ask them if it is possible to accommodate for that.
Often calling the restaurant will also help you figure out how seriously they take your intolerance and that can help you to decide whether you want to go there or not.
87. Pick dishes that look safe and make adaptations
If you come to a restaurant without calling beforehand, my strategy usually is to pick the dish that looks the safest. For example steak with fries and a salad.
Then I tell them about my intolerances, ask about the ingredients in the dish and ask them to swap certain ingredients if necessary.
Like this, you can create your own low FODMAP dish together with the restaurant staff.
88. Watch the amounts you eat
Overeating can cause symptoms in people with IBS. Therefore it is smart to also watch the amounts you eat when you eat out.
Try to eat slowly, chew well, and stop eating when you feel full. Of course, you won’t always manage to do this, but it is good to be aware of it.
89. It is a low FODMAP diet, not a no FODMAP diet
Keep in mind that this diet is about eating low in FODMAPs, not about not eating FODMAPs at all. This gives you a little bit more flexibility when you are in a restaurant.
Be careful with your trigger foods though, most people only need a tiny bit of garlic or onion to get symptoms.
90. Try a lactase supplement to better tolerate lactase
There are lactase supplements on the market that you can take when you eat a meal with lactose in it.
This supplement will help your body to break down the lactose, so you can eat the food without problems. This can be a lifesaver in a restaurant!
You can read more about how lactase supplements work in this blog.

91. Try a fructose supplement to better tolerate fructose
There are also supplements that help you to tolerate fructose better. You can read more about it in this blog.
92. Try a supplement to better tolerate fructans and galactans
Finally, there are also supplements to help you tolerate fructans (garlic, onion, wheat) and galactans (beans and pulses) better.
Also super helpful when you are eating out!
My favorite supplement for fructans and galactans is the Fibractase supplement by Intoleran. You can read more about this supplement in this blog.
Eating with friends and family
What if you have dinner at a friend’s house or a Christmas dinner with family? Below you can read my tips on how to navigate eating with family and friends:
93. Tell your loved ones about the diet
Please tell your family and friends about the diet and be honest about what the diet is for. It is crucial for you that you feel understood by the people around you.
I have written a script that can help you to tell your friends and family about the diet here.
94. Offer help when you are eating at somebody else’s place
If somebody who doesn’t know the FODMAP diet has to cook for you, they can feel overwhelmed. It is also difficult for them.
Therefore I always try to be helpful and offer help when I am going to eat at somebody else’s place. I offer to help them think of a recipe to cook, help them with preparing the food or bring some ingredients.
This makes it less daunting for both of you! You can find more tips for eating with friends in this blog.

95. Share low FODMAP recipes
My favorite thing to do is to just share a low FODMAP recipe that your host can prepare when they are cooking dinner (for example a recipe from my blog).
This makes things so much easier! It tells them exactly which ingredients to use and the end result will be low FODMAP. It is less of a hassle for them and feels more safe for you. Win-win!
96. Bring your own food
Is the host not willing to make an effort for you or do they really not understand the diet?
Then you can always bring your own food as a last resort. Not fun, but it will spare you a lot of stomach pain.
If the diet doesn’t work
The low FODMAP diet doesn’t work for everybody with IBS. If you have been following the elimination phase for 6 weeks and your symptoms haven’t settled down, the low FODMAP diet might not be the solution for you.
One of these tips can help you to take the next step:
97. Make sure that you were following the elimination phase correctly
Sometimes people keep having symptoms because they have accidentally been eating high-FODMAP foods during the elimination phase.
Work with a FODMAP-certified dietician and show him/her what you have been eating.
They can help to figure out if you have been making mistakes that could have caused symptoms.
98. Work with a gut-specialized doctor or dietician
If the tip above didn’t work and the diet doesn’t seem to work for you, it is important to visit a gastroenterologist doctor or gut-specialist dietician to help you figure out the next steps.
99. Try hypnotherapy
Hypnotherapy can improve IBS symptoms. A study by Monash University has shown that gut-directed hypnotherapy had a similar impact on IBS symptoms as a low FODMAP diet.
For some people following gut-directed hypnotherapy can really help to decrease their symptoms. Ask your doctor for advice before starting hypnotherapy.
A nice way to try gut hypnotherapy for a low price is the app Nerva. This is an IBS-focused hypnotherapy program created by a hypnotherapist from Monash University.
The final tip
If you have made it all the way to the bottom of this blog post: bravo! I hope that these tips have helped you on the way with the low FODMAP diet.
My final tip if there is anything more that you want to know:
100. Drop me a message!
If you have any questions left after reading this post, feel free to send me an email. Or leave a message in the Facebook group, there are always fodmappers there who will try to answer your questions.
I can’t help with any specialized questions regarding your health, because I am not a doctor or certified dietician, but I am an experienced fodmapper and I am always willing to answer questions about the diet!
For more blogs, recipes, and tips, you can also follow Karlijn’s Kitchen on social media:
Or subscribe to the newsletter below!
Together we go for a calm belly!
Subscribe to the Karlijn's Kitchen e-mail newsletter for more tips and recipes and receive the ebook 10 things I wish I had known when I started the FODMAP diet for free!
